Stool Chemistry
HSBTE DMLT IVth Semester. Stool Chemistry: Physical characteristics and chemical composition of stool, Detection of occult blood and excess fat in stool, Significance of blood and excess fat in stool.
BIOCHEMISTRY
Dr Pramila Singh
3/26/20247 min read
HSBTE. DMLT. IVth-Semester. Stool Chemistry: Physical characteristics and chemical composition of stool, Detection of occult blood and excess fat in stool, Significance of blood and excess fat in stool. Unit III. Biochemistry
Stool Chemistry
Stool chemistry is also known as stool analysis or fecal analysis. It involves the examination of the composition and characteristics of feces (stool). It gathers information about the digestive and absorptive functions of the gastrointestinal tract. Stool chemistry tests provide various aspects of gastrointestinal health. It is also used to diagnose or monitor certain medical conditions. Some important components of stool chemistry analysis are the Feacal Occult Blood Test (FOBT), Stool pH, Stool Culture, Fecal Fat Test (Quantitative and Qualitative), Fecal Elastase, Stool Color and Consistency, Ova and Parasite Examination, etc.
Physical characteristics and chemical composition of stool
Stool (feces or bowel movements) exhibits specific physical characteristics and chemical composition. Both the physical character and chemical composition of stool provide digestive and absorptive functions of the gastrointestinal tract. Both the physical and chemical properties of stool can be assessed through various analyses.
Physical Characteristics:
1. Color: Normal stool color varies from light to dark brown. It is due to the presence of bilirubin in stool. Bilirubin is a pigment formed during the breakdown of red blood cells. Changes in stool color indicate various conditions, such as bleeding (black, tarry stools), liver or gallbladder problems (pale or clay-colored stools), or dietary factors.
2. Consistency: Stool consistency ranges from hard and lumpy to soft and watery. The Bristol Stool Form Scale classifies stool into different types (ranging from Type 1, indicating constipation, to Type 7, indicating diarrhea). Changes in consistency are associated with dietary changes, hydration status, or underlying gastrointestinal conditions.
3. Shape: Normal stools have a formed appearance. Factors such as diet, hydration, and the presence of bowel obstructions cause Changes in stool shape.
4. Volume: Normal daily stool output varies among individuals. The increased volume may be associated with conditions like diarrhea or malabsorption. Decreased stool volume indicates constipation.
5. Odour: The odor of stool is primarily due to the action of gut bacteria on undigested food particles. Changes in stool odor may result from dietary variations or alterations in gut flora.
Chemical Composition
1. Water Content: The stool is composed of water, undigested food particles, bacteria, and waste products. The water content influences stool consistency. Higher water content contributes to softer stools.
2. Undigested Food Particles: Small amounts of undigested food, such as fibers and cellulose, are normally present in stool. Larger amounts may indicate malabsorption or rapid transit through the digestive tract.
3. Bacteria: A significant amount of bacteria are present in the large intestine. They contribute to the fermentation of undigested carbohydrates and the production of gases. Changes in bacterial composition affect stool odor and gas production.
4. Electrolytes: Stool contains electrolytes. These electrolytes include sodium, potassium, and chloride. Imbalances in electrolytes occur in conditions such as diarrhea or malabsorption.
5. Bile Pigments: Bilirubin, a breakdown product of haemoglobin. It gives stool characteristic brown color. Changes in bile production or flow affect stool color.
6. Fats: Small amounts of fats (lipids) are normally present in stool. Elevated levels may indicate malabsorption disorders, such as pancreatic insufficiency or celiac disease.
7. Mucus: Small amounts of mucus are normal in stool. Increased mucus production may be associated with inflammation or irritation of the gastrointestinal tract.
8. Blood: Occult blood in stool, not visible to the naked eye. It can be detected through laboratory tests. Visible blood may indicate bleeding in the gastrointestinal tract.
Detection of occult blood and excess fat in stool
1. Fecal Occult Blood Test (FOBT): FOBT is a common screening test that detects small amounts of blood in the stool that are not visible to the naked eye. This may indicate bleeding in the gastrointestinal tract. FOBT is carried out by the following methods.
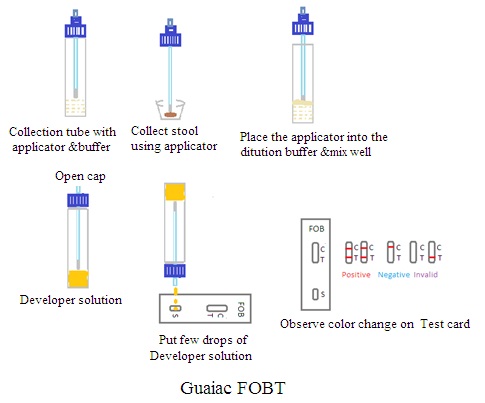
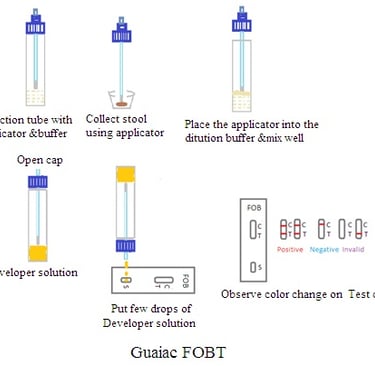
A. Guaiac FOBT:
Principle: It is a screening test. It involves applying a guaiac-impregnated paper to a stool sample. The guaiac reacts with the heme portion of hemoglobin in the blood. This causes a color change.
Materials Needed: Guaiac FOBT test kit, Disposable gloves, Collection stick or brush, Developer solution, Test cards, Plastic specimen container (optional), Paper towels or disposable pads, and Timer.
Procedure:
i.Preparation: Instruct dietary restriction to the patient to avoid constipation before the test. Set up a clean and well-lit workspace.
ii. Collection of Stool Sample: Provide written instructions to the patient on how to collect the stool sample. Instruct the patient to collect a small sample of stool using the collection stick or brush. Advise the patient to avoid contaminating the sample with urine or water. The patient should collect the sample directly into the container.
iii. Applying Sample to Test Card: Instruct the patient to apply a small amount of stool sample into the collection tube containing buffer solution. Mix well using the applicator. Apply a few drops of the sample mixture to the designated area on the test card. Ensure that the sample is spread evenly and covers the entire area.
iv. Developing the Test: Apply a few drops of developer solution to the area of the test card containing the stool sample using the dropper provided with the kit. Allow the developer solution to react with the sample. This involves waiting a specific amount of time (e.g., 1-2 minutes).
v.Interpretation of Results: Visually inspect the test card for any color changes. A blue color change indicates a positive result. It suggests the presence of blood in the stool. A negative result is indicated by the absence of any color change.
vi. Documentation and Reporting: Record the results accurately, including the patient's details and the date and time of the test. Provide the results to the healthcare provider.
vii. Disposal: Safely dispose of all used materials according to medical waste disposal guidelines.
Benzidine test for FOBT
This test is a screening method used to identify the presence of blood in the stool. It indicates various gastrointestinal conditions, including colorectal cancer.
Principle: Benzidine is a chemical compound that undergoes a color reaction in the presence of hemoglobin. Benzidine reacts with the heme portion of hemoglobin to produce a blue-green color. The reaction occurs due to the oxidation of benzidine by the peroxidase activity of hemoglobin in the presence of hydrogen peroxide. The intensity of the color change depends on the amount of blood present in the sample.
Materials Needed: Benzidine reagent solution, Hydrogen peroxide solution, Disposable gloves, Collection stick or brush, Test cards or filter paper, Disposable containers or wells, Paper towels or disposable pads, Timer
Procedure:
i. Preparation: Instruct dietary restriction to the patient to avoid constipation prior to the test. Set up a clean and well-lit workspace.
ii. Collection of Stool Sample: Provide written instructions to the patient on how to collect the stool sample. Instruct the patient to collect a small sample of stool using the collection stick or brush. Advise the patient to avoid contaminating the sample with urine or water. The patient should collect the sample directly into the container.
iii. Applying Sample to Test Card: Instruct the patient to apply a small amount of stool sample to the designated area on the test card. Ensure that the sample is spread evenly and covers the entire area.
iv. Benzidine Reaction:
a. Place a few drops of benzidine reagent solution into a clean, disposable container or well.
b. Add a drop of hydrogen peroxide solution to the container or well containing the benzidine reagent.
c. Mix the solutions gently using a clean applicator stick or pipette.
d. Immediately apply the benzidine reagent solution to the glass slide containing the stool sample. Ensure that the benzidine reagent solution completely covers the sample area.
e. Allow the reaction to proceed. This involves waiting for a specific amount of time (e.g., 1-2 minutes).
v. Interpretation of Results: Visually inspect the test card for any color changes after the specified development time. A blue-green color change indicates a positive result. It suggests the presence of blood in the stool. A negative result is indicated by the absence of any color change.
vi. Disposal: Safely dispose of all used materials according to medical waste disposal guidelines.
vii. Documentation and Reporting: Record the results accurately, including the patient's details and the date and time of the test. Provide the results to the healthcare provider.
viii. Disposal: Safely dispose of all used materials according to medical waste disposal guidelines.
2. Detection of Excess Fat in stool:
Excess fat in stool is called steatorrhea. Steatorrhea is important for diagnosing various gastrointestinal disorders such as malabsorption syndromes, pancreatic insufficiency, or liver diseases.
Principles: Excess fat in stool is identified by the qualitative test of fecal fat. Normally, feces contain small amounts of fat. However, an increase beyond a certain threshold indicates malabsorption of fats in GIT. Sudan III dye is used. It stains fat globules to develop a red-orange color.
Procedure:
i.Stool Sample Collection: Instruct the patient to collect a fresh stool sample in a clean, dry container. Ideally, collect samples over 72 hours to get a more accurate representation of fat excretion.
ii. Qualitative Tests:
Gross Examination: Visual inspection of the stool for greasiness, oiliness, or floating characteristics provides information about the presence of fat in the stool.
Sudan III Stain: Sudan III dye is used for the qualitative test of fat in stool. Prepare stool smear on a dry clean slide. Add Sudan III dye to the stool sample smear. The dye binds to fat globules to develop red orange color in the fat present in the stool sample. Examine fat droplets stain red-orange under microscopic. The presence of a significant amount of red-stained fat globules indicates excess fat in the stool
iii. Additional Tests:
Stool pH: Alkaline stool pH (above 7) may suggest malabsorption of fat.
Stool Microscopy: Examination for undigested food particles, muscle fibers, or fat globules under the microscope.
Significance of the presence of blood and excess fat in stool
The presence of blood and excess fat in stool has significant clinical implications. It indicates underlying health conditions.
Clinical Significance of Presence of Blood in Stool:
1. Gastrointestinal Bleeding: Visible or occult blood in the stool suggests gastrointestinal bleeding.
Possible Causes: Peptic ulcers, Gastritis, Colorectal polyps or cancer, Inflammatory bowel disease (e.g., Crohn's disease, ulcerative colitis). Gastrointestinal infections, etc
2. Colorectal Cancer Screening: Fecal Occult Blood Tests (FOBT or iFOBT) are commonly employed for routine colorectal cancer screening.
3. Upper Gastrointestinal Bleeding: Black, tarry stools (melena indicate upper gastrointestinal bleeding.
Possible Causes: Peptic ulcers in the stomach or duodenum, Esophageal varices, Mallory-Weiss tear
Presence of Excess Fat in Stool
1. Malabsorption Disorders: Elevated levels of fat in the stool indicate malabsorption of dietary fats.
Possible Causes
· Pancreatic insufficiency: Impaired production of digestive enzymes by the pancreas.
· Celiac disease: Gluten intolerance leading to damage to the small intestine.
· Crohn's disease: Inflammatory bowel disease affecting the digestive tract.
2. Steatorrhea: Excessive fat in the stool, known as steatorrhea. It results in foul-smelling, greasy stools.
Clinical Indication: Helps diagnose and differentiate conditions causing malabsorption.
3. Pancreatic Disorders: Fat malabsorption is associated with pancreatic disorders.
Possible Causes: Chronic pancreatitis, pancreatic cancer, Cystic fibrosis
4. Celiac Disease: Gluten-induced damage to the small intestine is celiac disease. It leads to malabsorption of nutrients, including fats.
5. Inflammatory Bowel Disease: Conditions like Crohn's disease or ulcerative colitis affect the absorption of nutrients, including fats.
Dr Pramila Singh
