Haemostasis
Haemostasis: 1.1 Introduction to normal hemostasis. 1.2 Theories of blood coagulation. 1.3 Platelets and their role in haemostasis including count. 1.4 Bleeding disorders and related diseases. 1.5 Principles, clinical importance, reference values and methods of: prothrombin time, prothrombin time index (PTI) International normalized ratio (INR), Activated Partial Thromboplastin time (APTT), Thrombin Time (TT), bleeding time (BT), Hess test, clotting time (CT), and clot retraction test (CRT).
HAEMATOLOGY
Dr Pramila Singh
2/18/202416 min read
HSBTE DMLT IV Semester Unit-I: Hemostasis: Introduction to normal hemostasis. Theories of blood coagulation. Platelets and their role in hemostasis including count. Bleeding disorders and related diseases. Principles, clinical importance, reference values, and methods of prothrombin time, prothrombin time index (PTI) International normalized ratio (INR), Activated Partial Thromboplastin time (APTT), Thrombin Time (TT), bleeding time (BT), Hess test, clotting time (CT), and clot retraction test (CRT).
Hemostasis is the physiological process that prevents and stops bleeding and maintains the circulatory system. It maintains a balance between preventing excessive bleeding (hemorrhage) and avoiding unnecessary blood clotting (thrombosis). Normal hemostasis is essential for the maintenance of vascular health and preventing pathological conditions.
Disorders of Hemostasis
1. Hemorrhagic Disorders:
Thrombocytopenia: Low platelet count.
Hemophilia: Deficiency of clotting factors.
2. Thrombotic Disorders:
Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE): Abnormal clot formation.
Disseminated Intravascular Coagulation (DIC): Widespread activation of coagulation.
Theories of blood coagulation
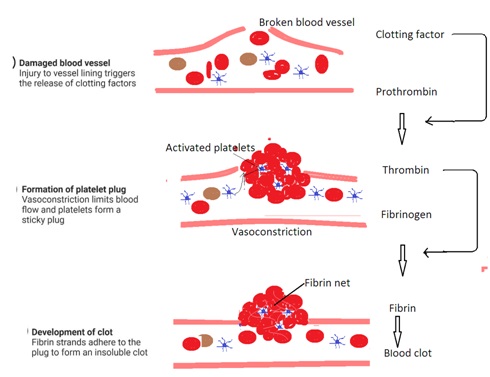
Blood coagulation is a process of blood clot formation. It is a complex and highly regulated physiological process that prevents excessive bleeding after injury. Two theories the Contact Activation Theory and the Tissue Factor Pathway explain blood coagulation.
1. Contact Activation Theory:
Intrinsic Pathway: It is also known as the contact activation pathway. This theory suggests that clotting is initiated by disturbance inside the vascular system.
Contact Factor: These include factors XII, XI, IX, and VIII.
Platelets: Platelets play a role in the activation and amplification of the coagulation.
Steps
· Initiation: After blood vessel injury, blood comes into contact with negatively charged surfaces (collagen).
· Contact Activation: Factor XII (Hageman factor) comes into contact with the exposed collagen and becomes activated.
· Intrinsic factor activation: Activated factor XII triggers a cascade of reactions. This leads to the activation of factors XI, IX, and VIII.
· Amplification: Activated factor IX, along with factor VIII and platelets, forms the tenase complex, amplifying the coagulation cascade,
· Common Pathway: The intrinsic pathway merges with the extrinsic pathway to activate factor X. This leads to the formation of the prothrombinase complex and the conversion of prothrombin to thrombin.
· Fibrin Formation: Thrombin converts fibrinogen into fibrin strands, and Fibrin forms a clot.
2. Tissue Factor Pathway (Extrinsic Pathway):
Extrinsic Pathway: This theory suggests that clotting is initiated by external trauma. This leads to the release of tissue factor (TF).
Tissue Factor (TF): Tissue factor substance released by damaged tissues that initiate the clotting cascade.
Extrinsic Pathway Factors: This includes factors VII, III (tissue factor), and Ca²⁺.
Steps
1. Tissue Injury: External trauma exposes tissue factor (TF).
2. TF Activation: TF interacts with factor VII, activating it.
3. Extrinsic Pathway Activation: Activated factor VII, along with tissue factor, activates factor X.
4. Common Pathway: The intrinsic pathway merges with the extrinsic pathway at the activation of factor X.
5. Prothrombinase Complex: Factor X combines with factor V, This combination forms the prothrombinase complex.
6. Thrombin Formation: Prothrombinase converts prothrombin to thrombin.
7. Fibrin Formation: Thrombin converts fibrinogen into fibrin strands, leading to clot formation.


Platelets and their role in hemostasis including count.
Platelets or thrombocytes are one of the cellular components of blood. Platelets are small, disc-shaped blood cells without a nucleus. They play an important role in the complex process of hemostasis. Hemostasis is the process of preventing and stopping bleeding.
Platelet Counts: The normal range for platelet count in a healthy individual is between 150,000 and 450,000 platelets per microliter of blood. Abnormal platelet counts indicate various medical conditions. Low platelet counts (thrombocytopenia) indicate a risk of increased bleeding and high platelet counts (thrombocytosis) indicate a risk of blood clotting disorders.
Platelets' role in hemostasis: Platelets respond quickly to vascular injury. Platelets adhere to damaged areas, release chemicals, form a temporary plug, and contribute to the coagulation cascade. Maintaining an appropriate platelet count is essential for ensuring effective hemostasis and preventing bleeding or clotting disorders.
1. Vascular Spasm:, Platelets contribute to vasoconstriction, minimizing blood flow and reducing initial blood loss after injury to a blood vessel.
2. Platelet Adhesion: Platelets adhere to the exposed collagen fibers at the site of injury. This initiates the hemostatic response.
3. Platelet Release Reaction:, Platelets undergo a release reaction after adhesion with injured blood vessels. They release stored chemicals such as ADP, serotonin, and thromboxane A2. These substances enhance vasoconstriction, attract more platelets, and stimulate the formation of a platelet plug.
4. Platelet Aggregation: Released substances promote platelet aggregation. This leads to the formation of a temporary platelet plug that seals small breaks in the injured blood vessel.
5. Coagulation Cascade: Platelet release factors activate the coagulation cascade. The coagulation cascade is a series of biochemical reactions that result in the conversion of fibrinogen to fibrin threads. Fibrin threads strengthen the platelet plug by forming a more stable blood clot.
6. Clot Retraction and Repair: Platelets contract and contribute to clot retraction, pulling torn areas of the blood vessel together to facilitate repair.
7. Fibrinolysis: The blood clot is gradually dissolved through fibrinolysis after blood vessels heal. Plasmin, an enzyme, breaks down fibrin, allowing for the restoration of normal blood flow.

Bleeding disorders and related diseases
Bleeding disorders include abnormalities in the blood clotting process. The blood clotting mechanism is also known as hemostasis. Hemostasis involves complex interactions between platelets, proteins, and other blood components. The following are some bleeding disorders
1. Hemophilia: Hemophilia is a genetic disorder characterized by a deficiency or absence of clotting factors, such as factor VIII (hemophilia A) or factor IX (hemophilia B). Their absence stops blood clotting and results in prolonged bleeding.
2. Thrombocytopenia: Thrombocytopenia is a condition characterized by a low platelet count. Platelets are essential for the initial stages of blood clotting. A low platelet count leads to spontaneous bleeding or excessive bleeding following minor injuries. Thrombocytopenia can be caused by various factors, including immune disorders, medications, infections, and certain medical conditions.
3. Vitamin K Deficiency: Vitamin K is crucial for the synthesis of clotting factors in the liver. Deficiency in vitamin K leads to impaired blood clotting and excessive bleeding. Intestinal bacteria are responsible for vitamin K production. Newborns are susceptible to vitamin K deficiency because newborn intestinal bacteria are not fully developed.
4. Liver Disease: The liver produces many clotting factors. Liver diseases such as cirrhosis result in decreased synthesis of these factors. This leads to a bleeding tendency.
5. Hematologic Cancers: Cancers that affect the blood, such as leukemia and lymphoma, interfere with normal blood clotting. These conditions lead to abnormal bleeding or clotting.
6. Intravascular Coagulation: It is a serious condition where the clotting process is activated throughout the body. This leads to the formation of numerous blood clots. This leads to organ damage, as well as excessive consumption of clotting factors. Excessive consumption of clotting factors leads to bleeding. DIC is often associated with severe infections, trauma, or certain medical conditions.
7. Von Willebrand Disease (VWD): Von Willebrand disease is the most common inherited bleeding disorder. It is caused by a deficiency or dysfunction of von Willebrand factor (vWF). Willebrand factor (vWF) is a protein that plays a crucial role in platelet adhesion and the clotting process. Individuals with VWD may experience easy bruising, prolonged bleeding after injuries, and, in women, heavy menstrual bleeding.
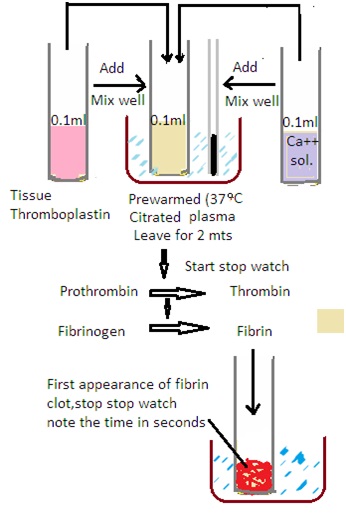
Principles, clinical importance, reference values, and methods of prothrombin time
Principles: The time required to clot blood plasma after bleeding is called Prothrombin time (PT). During blood coagulation, Prothrombin forms thrombin in the presence of thromboplastin and calcium. Fibrinogen form fibrin. They form blood clots. The time required for the blood plasma to clot is measured in seconds.
Clinical Importance
1. Warfarin Monitoring: PT is frequently used to monitor patients on oral anticoagulant therapy, especially warfarin. PT provides an indication of warfarin's effectiveness.
2. Screening for Coagulation Disorders: PT is part of the coagulation profile. It includes a routine screening to detect abnormalities in the clotting cascade. It helps to identify conditions such as vitamin K deficiency or clotting factor deficiencies.
3. Liver Function Assessment: PT is sensitive to the levels of clotting factors produced by the liver. Liver diseases, such as cirrhosis, lead to a decrease in the synthesis of clotting factors. This results in an increased PT.
4. Preoperative Assessment: PT is used as a part of preoperative assessments to evaluate a patient's bleeding risk during surgery.
Reference Values: The reference values for prothrombin time can vary slightly. It depends on the laboratory and the reagents used. However, a commonly accepted reference range is approximately 11 to 13 seconds. Results are often reported as the patient's PT compared to a control or as an International Normalized Ratio (INR).
Method:
Several methods are used to perform the PT test, but the basic principles remain the same.
1. Add 0.1 mL prewarmed plasma up to 37 degrees C in a clean test tube,
2. Add 0.1 ml tissue thromboplastin. Mix well and Set-a-side for two minutes at 37 degrees C,
3. Add 0.1 mL Calcium chloride solution into the plasma. Mix well and start the stopwatch.
4. Observe the clotting process and stop the stopwatch on the appearance of fibrin in a test tube.
Report the result in seconds.

Principles, clinical importance, reference values, and methods of prothrombin time index (PTI)
Principle: Prothrombin Time (PT) is a laboratory test that measures the time it takes for blood to clot. PTI, or Prothrombin Time Index is a normalized value derived from PT. The test assesses the functionality of the extrinsic pathway and common coagulation pathways. It primarily reflects the activity of factors I (fibrinogen), II (prothrombin), V, VII, and X. PTI is expressed as a percentage, representing the patient's clotting time compared to a standardized control.
Clinical Importance:
1. Monitoring Warfarin Therapy: PTI is commonly used to monitor patients on oral anticoagulant therapy, such as warfarin. The goal is to maintain the PTI within a therapeutic range, preventing both excessive bleeding and insufficient anticoagulation.
2. Liver function Test: PTI is sensitive to changes in certain clotting factors produced by the liver (factors II, V, VII, and X). Elevated PTI can indicate liver dysfunction.
3. Coagulation Disorder Detection: Abnormal PTI values may suggest inherited or acquired coagulation disorders, including vitamin K deficiency or disseminated intravascular coagulation (DIC).
Reference Values: The reference range for PTI is between 70% and 130%. The specific range may vary slightly among different laboratories.
Methods: The PTI is calculated by dividing the patient's PT by the mean normal PT and then multiplying by 100. The formula is as follows
PTI = (patient's PT/ mean normal PT) X 100.
1. Patient's PT: The time in seconds. Time in seconds is required for the patient's blood to clot.
2. Mean normal PT: The average PT of a group of healthy individuals. This value serves as the reference point for normal clotting time.
Laboratory Methods: PT is measured using a coagulation analyzer. The test involves adding tissue factor and calcium to the patient's plasma. This initiates the extrinsic pathway. The time taken for clot formation is then measured.
Principles, clinical importance, reference values, and methods of International normalized ratio (INR).
Principle: The International Normalized Ratio (INR) is a standardized measurement of blood clotting time, derived from the prothrombin time (PT) test. INR is used to monitor and adjust the dosage of oral anticoagulant medications, such as warfarin. Standardization is necessary because different laboratories may use different reagents and methods for PT. INR ensures consistency in interpreting the results.
Clinical Importance:
1. Warfarin Monitoring: INR is crucial for monitoring patients on oral anticoagulant therapy, such as warfarin. Maintaining the INR within a target range is essential to balance the risk of bleeding and the risk of thrombosis.
2. Prothrombotic Conditions: INR monitoring is also relevant in assessing individuals with prothrombotic conditions It ensures appropriate anticoagulation to prevent clot formation.
3. Prevent Blood Clot: INR testing helps prevent the formation of abnormal blood clots, reducing the risk of conditions like deep vein thrombosis (DVT), pulmonary embolism (PE), and stroke.
Reference Values: The INR values vary depending on the medical condition and the effect of anticoagulation. However, a common INR range for patients on warfarin therapy is 2.0 to 3.0. For certain conditions, such as mechanical heart valves, higher ranges may be recommended.
Method: The INR is calculated using the following formula
INR = (Mean Normal PT/Patient’s PT)ISI
· Patient’s PT: The time, in seconds required for the patient's blood to clot. It is determined through the PT test.
· Mean Normal PT: The average PT of a group of healthy individuals.
· International Sensitive Index (ISI): A calibration factor specific to the thromboplastin reagent used in the PT test. It accounts for variations in sensitivity between different reagents.
Laboratory Method: Laboratories measure PT using a coagulation analyzer and a specific thromboplastin reagent. The result is then used in the INR formula to standardize the PT values. The use of the ISI ensures consistency across different reagents and instruments.
Principles, clinical importance, reference values, and methods of Activated Partial Thromboplastin time (APTT).
Principle: Activated Partial Thromboplastin Time (APTT) is a laboratory test that measures the time for blood to clot through the intrinsic pathway and common coagulation pathways. It assesses the activity of various coagulation factors, including factors VIII, IX, XI, and XII, as well as common pathway factors (X, V, II, and I). APTT is activated by a substance known as an activator and calcium. An activator and calcium mimic the activation of clotting.
Clinical Importance:
1. Monitoring Heparin Therapy: APTT is commonly used to monitor patients undergoing anticoagulant therapy with heparin. The test helps ensure that the heparin dosage is within the therapeutic range, preventing both excessive bleeding and insufficient anticoagulation.
2. Detection of Coagulation Disorders: APTT is sensitive to deficiencies or abnormalities in intrinsic and common pathway coagulation factors. It is used to detect and evaluate conditions such as hemophilia, von Willebrand disease, and other inherited or acquired bleeding disorders.
3. Assessment of Liver Function Test: Liver-produced clotting factors for the intrinsic pathway. This influences APTT. Abnormalities in APTT can indicate liver dysfunction.
Reference Values: The reference range for APTT is typically between 25 to 35 seconds. However, specific reference values can vary among laboratories.
Methods: The APTT test involves the following steps
1. Sample Collection: Blood is drawn from the patient, and the plasma is separated from the blood cells.
2. Activation: The intrinsic pathway is activated by adding an activator (such as kaolin) to the plasma sample. This initiates the coagulation cascade.
3. Calcium Addiction: Calcium is then added to the mixture to facilitate the coagulation process.
4. Clot Detection: The time required for the clot to form is measured and reported as the APTT.
Principles, clinical importance, reference values, and methods of Thrombin Time (TT).
Principles: Thrombin Time (TT) is a laboratory test to measure the time required for a fibrin clot to form after the addition of thrombin to plasma. Thrombin is an enzyme critical for the conversion of fibrinogen to fibrin. It is the final step in the coagulation cascade. TT primarily assesses the functionality of fibrinogen and the conversion to fibrin
Clinical Importance:
Fibrinogen Assessment: TT is used to evaluate the functional integrity of fibrinogen. Fibrinogen is a plasma protein essential for blood clot formation. Abnormal TT results indicate abnormalities in fibrinogen concentration or function.
1. Detection of Fibrinolytic Disorders: TT can be useful in assessing fibrinolysis. the process of breaking down fibrin clots. Prolonged TT may suggest a potential fibrinolytic disorder.
2. Monitoring Heparin Therapy: In some cases, TT may be used to monitor the effects of heparin therapy. It is used in situations where conventional tests like APTT are not suitable.
Reference Values: The reference range for TT is between 14 to 16 seconds. However, specific reference values vary among laboratories.
Methods: The Thrombin Time test involves the following steps.
1. Sample Collection: Blood is drawn from the patient, and the plasma is separated from the blood cells.
2. Thrombin Addition: Thrombin, a coagulation enzyme, is added to the plasma sample.
3. Clot Detection: The time it takes for a fibrin clot to form is measured in seconds and reported as the Thrombin Time.
4. Interpretation: A normal TT indicates that fibrinogen is functioning correctly and be converted to fibrin. Prolonged TT suggests a deficiency or dysfunction of fibrinogen
Dr Pramila Singh


Principles, clinical importance, reference values, and methods of bleeding time (BT).
Principles: Bleeding Time (BT) is a test to assess the hemostasis. Duke’s method and Ivy’s method are used to measure bleeding time. Cut on the upper arm is made to measure bleeding time in Ivy’s method. The ear lobe or fingertip is pricked to measure bleeding time in Duke’s method. The ear lobe is a better choice than the tip
. Reason: Earlobe is more vascular and has more subcutaneous tissues than fingertips. Thus blood flow in the earlobe is better than in the fingertip.
Clinical Importance:
BT test informs the ability of platelets to adhere to the blood vessel wall, form a plug, and stop bleeding from a small, incision. It provides information about the initial phase of blood clotting and platelet function.
1. Platelet Function Assessment: BT is used to evaluate platelet function. Prolonged bleeding time indicates disorders affecting platelet adhesion and aggregation, such as von Willebrand disease or platelet function disorders.
2. Preoperative Screening: BT is used as a part of preoperative screening to assess a patient's bleeding risk before surgery. However, its use has diminished in recent years due to the availability of more specific and standardized tests.
3. Qualitative Platelet Disorders: BT can help identify qualitative platelet disorders, where the structure or function of platelets is abnormal. Such as thrombocytopenia, acute leukemia, aplastic anemia, liver diseases, etc.
Reference Values: The reference range for bleeding time is between 2 to 9 minutes. However, specific reference values can vary among laboratories and methods used.
Duke’s Methods:
The Bleeding Time test involves the following steps
Patient Preparation: The patient is asked to stop taking medications that affect platelet function, such as aspirin, for a specified period before the test.
1. Prick: Sanitize the ear lobe/fingertip using a spirit swab. Use a sterile lancet to make about 3 mm deep puncture.
2. Blood Collection: Start the stopwatch on the appearance of blood. Wipe off blood using blotting paper at 30-second intervals. Note down the time required to stop bleeding. The time for bleeding to stop is measured in minutes and seconds.
Result: Normal bleeding time 1 to 6 minutes.


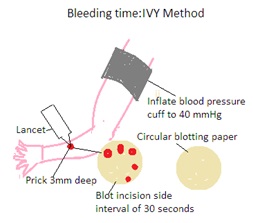

Ivy’s Method:
The result of Ivy’s method is more accurate than Duke’s method.
1. Patient Preparation: The patient is asked to stop taking medications that affect platelet function, such as aspirin, for a specified period before the test.
2. Sphygmomanometer (BP Apparatus): Wrap the Sphygmomanometer cuff on the Patient's upper arm (forearm). Inflate it to maintain a pressure of 40 mm of mercury during the test.
3. Incision: Sanitize the skin surface. Use a sterile lancet to make it 3 mm deep. Maintain a gap of 5 to 10 cm between two incisions.
4. Blood Collection: Start the stopwatch just on the appearance of blood. Wipe off blood using blotting paper at 30-second intervals. Note down the time required to stop bleeding at both incisions. The time for bleeding to stop is measured in minutes and seconds.
Result: Normal bleeding time: 2 to 8 minutes
Interpretation: Prolonged bleeding time suggests a defect in hemostasis. It is normally related to platelet dysfunction.
Principles, clinical importance, reference values, and methods of Hess test.
The Hess test is also known as the Rumpel-Leede test, Tourniquet test, or Capillary Fragility Test. The Hess test assesses capillary fragility and vascular integrity. It is used in the context of bleeding disorders and certain medical conditions.
Principle: The Hess test evaluates capillary fragility by applying a tourniquet or blood pressure cuff to a patient's arm for 10 minutes. This induces venous stasis. Petechiae (small, pinpoint hemorrhages) may appear on the patient's skin. It is mainly due to poor platelet functioning. It indicates increased capillary fragility.
Clinical Importance: It is used to assess the capillary fragility and vascular integrity in patients with bleeding disorders or suspected vascular abnormalities.
Reference Values: There should be no or less than 10 petechiae in one square meter area after the release of the tourniquet.
Method:
1. Measure the systolic and diastolic blood pressure of the patient.
2. Apply a blood pressure cuff and inflate the pressure higher than the systolic blood pressure for 5 minutes.
3. After releasing the cuff, the appearance of petechiae is observed.
These tests are not specific and may be affected by various factors. Interpretation should be done in conjunction with the patient's clinical history, symptoms, and other laboratory investigations. Abnormal results may suggest capillary fragility or other vascular abnormalities that warrant further investigation.






Principles, clinical importance, reference values, and methods of clotting time (CT),
Principle: Clotting time refers to the time it takes for blood to form a stable clot after initiation of the coagulation cascade. It assesses the overall efficiency of the intrinsic and common pathways of the coagulation cascade. Clotting time is affected by factors such as the concentration of clotting factors, platelets, and the presence of inhibitors.
Clinical Importance:
· Clotting time is a broad measure of the coagulation process and is used in the initial assessment of bleeding disorders.
· It helps in detecting deficiencies or abnormalities in clotting factors, which may lead to prolonged bleeding times.
· Clotting time can be indicative of liver disease, vitamin K deficiency, and certain hereditary clotting factor deficiencies.
Reference Values: Normal clotting time can vary depending on the specific method used, but it typically falls within the range of 8 to 15 minutes.
Methods:
· Lee-White Method:
· Make a venepuncture and withdraw 5 mL blood using a siliconized dry glass syringe/ disposal plastic syringe.
· Select three 8 X 75 mm test tubes and deliver one mL of blood in each test tube.
· keep test tubes in an upright position in a water bath and maintain a temperature of 37 degrees C.
· Tilt each test tube to ascertain blood coagulation. The first tube is gently tilted every minute and the remaining test tubes are examined every half minute.
· Note down the average clotting time.
normal Range:5 to 10 minutes
· Capillary Tube Method: It is performed when venous blood is not available. It is a less sensitive and unreliable method
· Clean fingertip using a spirit swab.
· Make a 3 mm deep puncture using a sterile needle.
· Wipe off the first drop and fill blood into two capillary tubes. After two minutes break the capillary tube to chick fibrin thin thread.
Break the capillary tube repeatedly till the formation
· Automated Coagulation Analyzers: Modern laboratories often use automated instruments that can measure clotting time as part of a panel of coagulation tests. These instruments provide more accurate and standardized results.
The results may be affected by various factors, including temperature, the presence of anticoagulants, and the specific reagents used in the testing method. Clotting time is a relatively basic coagulation test, and more specific tests, such as prothrombin time (PT) and activated partial thromboplastin time (aPTT), are often employed for a more detailed assessment of coagulation pathways. Interpretation of clotting time results should be done in the context of the patient's overall clinical condition and other laboratory findings.
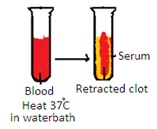
CLOT RETRACTION TIME TEST (CRT)
Qualitative Method
1. Collect 5 to 10 mL of venous blood in a clean test tube,
2. Heat it to 37 degrees C in a water bath
3. Observe clot retraction
4. Normal range: 4 hours for complete retraction
Quantitative method
1. Calculate the hematocrit value of patient blood.
2. Collect 5 to 10 mL venous blood in a centrifuge tube containing 2 mL EDTA.
3. Put the applicator stick into a centrifuge tube.
4. Put the centrifuge tube in a water bath maintaining a temperature of 37 degrees C for one hour.
5. Remove the applicator stick with blood clots from the centrifuge tube. Allow serum to remain in a centrifuge tube.
6. Not down blood clot condition: firm or friable, complete retraction or poor retraction.
7. Measure the serum volume in a centrifuge tube.
Calculation:
Clot retraction = Serum volume X 10/ 100 – Haemtocrit%
Clot retraction % = Clot retraction X 100.
Normal Range: 58 to 97% in one hour.
Clinical importance: Delayed CRT indicates Thrombocytopenia, Polycythemia, Thrombosthenia, Haemophilia, Hypofibrinogenemia, and Dysfibrinogenemia.