Gram Negative bacteria
Characteristics, antibiotics related to Gram Negative bacteria, and their distribution: Pseudomonas, Proteus, Vibrio Cholerae, Neisseria, Treponema Pallidium. Unit II 2.6 Mycobacterium tuberculosis and leprae.
Dr Pramila Singh
2/29/20248 min read
Characteristics, antibiotics related to Gram-negative bacteria, and their distribution: Pseudomonas, Proteus, Vibrio cholerae, Neisseria, Treponema pallidium. Unit II
The cell wall of gram-negative bacteria has a small amount of peptidoglycan. The outer layer of the cell wall has toxic lipopolysaccharide. This lipopolysaccharide acts as an endotoxin.
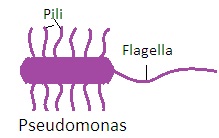
2.1 PSEUDOMONAS
There are several species of pseudomonas. Followings are some medically important Pseudomonas: Pseudomonas aeruginosa. Pseudomonas maltopholia, Pseudomonas cepacia,, Pseudomonas alcaligens, Pseudomonas fluorescens.
1. Characteristics of Pseudomonas:
i. Aerobic, non-sporting, motile, Gram-negative rod bacteria with polar flagella.
ii. Ferment carbohydrates by oxidation to derive energy
iii. Catalase positive, Oxidase Positive, Arginine hydrolysis positive,
iv. H2S negative, indol negative, MR negative, VP negative,
v. Reduces nitrate to nitrite.
vi. Grow in simple culture media with a characteristic smell.
vii. Inoculated culture media may be pigmented to develop blue-green color.
viii. Habitat: They require little nutrients to grow. Water, soil, sewage in humid areas, rice paddy fields, river banks, and stagnant water surface.
ix. Pathogenicity:
· They are opportunistic bacteria that cause nosocomial infections.
· In hospitals they cause local infections in the urinary tract, respiratory tract, eye, external and middle ear, burns, and wounds.
· They cause septicemia and infantile diarrhea.
· Its ability to grow in simple aqueous media contaminates distilled water, intravenous fluid, and equipment in hospitals related to respiratory therapy and anesthesia.
· They produce both endotoxin and exotoxin. Exotoxin inhibits protein synthesis in the human body.
x. Culture media requirements: Simple or enriched culture media. MacConkey agar culture media is the most preferred culture media. Growth temperature ranges from 4 degrees C to 45 degrees C. The optimum temperature for growth is 37 degrees C.
xi. Colony: Large, circular, irregular or entire margin, flat, soft, opaque, green pigmentation in culture media, Grape-like or musty smell.
xii. Biochemical characteristics:
1Citrate: Positive
2. Gelatine: Positive
3. Nitrate: Positive
4. Oxidase: Positive
5 MR: Negative
6. VP: Negative
7. Indole: Negative
xiii. Sugar Fermentation
1. Glucose: Positive, It is due to oxidation, not fermentation
2. Lactose: Negative
3. Sucrose: Negative
4. Maltose: Negative
5. Xylose: Negative
6. Mannitol: Negative
2. Antibiotics related to Pseudomonas: Sensitive to aminoglycosides, some cephalosporins, some penicillins, and polymixins. Resistant to most commonly used antibiotics.
3. Distribution of Pseudomonas: They are saprophytes and require little nutrients to grow. found in soil, sewage, organic wastes, sinks, humidifiers, warm moist areas, rice paddy fields, river banks, and stagnant water.
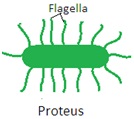
2.2 PROTEUS
There are four species of the genus Proteus. These are Proteus vulgaris, Proteus mirabilis, Proteus stuartii, Proteus morganii. Now only Proteus vulgaris is considered as Proteus. Others have been shifted to another genus of bacteria.
1. Characteristics of Proteus:
i. Motile, non-spore-forming, non-capsulated, rod-shaped with variable length, Gram-negative bacteria.
ii. Culture media requirements: Simple nutrient culture media, enteric culture media, MacConkey,s agar culture media, Eosin methyl blue agar culture media.
iii. Colony: Circular, diameter 1mm, entire margin, slight elevation, soft, translucent with fishy or ammonical odor. on overnight incubation at 37o C.
iv. Pathogenicity: Infection in the urinary tract, wound, chest, and septicemia.
v. Fermentation characteristics: do not ferment lactose
1. Glucose: Positive
2. Xylose: Positive
3. Sucrose: Positive
4. Maltose: Positive, Release acid with gas
5. Lactose: Negative
6. Mannose: Negative
7. Mannitol: Negative
vi. Biochemical characteristics
1MR: Positive
2 Urease: Positive
3. Indole: Positive
4. Gelatin: Positive
5. Nitrate: Positive
6. PPA: Positive
7. VP: Positive
8. KCN: Positive
9. H2S: Positive
10. Oxidase: Negative
11. TSI: Base: Acid, Slant: Acid with release of gas
2. Antibiotics related to Proteus: Sensitive to aminoglycosides and cephalosporins. Resistant to tetracycline and polymixins.
3. Distribution of Proteus: Human and animal intestine, water. soil and sewage.
VIBRIO CHOLERAE
Vibrio cholerae does not belong to the family Enterobacteriaceae but it causes enteric diseases such as cholera. It belongs to the family Vibrianaceae.
1. Characteristics of Vibrio cholerae:
i. Curved, “coma-shaped” single polar flagellated, highly motile, Gram-negative rods, aerobic and facultative anaerobic bacteria,
ii. Non-spore forming. (Asporogenous),
iii. Mostly non-capsulated
iv. Culture media requirements: MacConkey agar culture media, incubation period 24 hours, and optimum temperature 370C. Other suitable culture media are thiosulphate-citrate-bile salt sucrose agar culture media and alkaline peptone water containing 10g/L sodium chloride culture media.
v. Colony: Circular with diameter 1 mm, entire margin, flat elevation, colorless becomes reddish on prolonged incubation, opaque and soft.
vi. Pathogenicity: Vibrio cholerae is transmitted by fecal contamination of water and food. Human carriers are normally asymptomatic. Poor sanitation, malnutrition, overcrowding, and inadequate medical facilities contribute to the spread of cholera. Patient quarantine does not prevent cholera because most humans are asymptomatic.
Vibrio cholerae is stomach acid sensitive. Thus, the entry of more than 1 billion Vibrio cholera into GIT develops cholera. Individuals with no stomach acid or on antacid therapy are more susceptible to Vibrio cholera. Vibrio cholera adheres with the GIT mucus membrane and secretes enterotoxin known as cholerogen. Cholerogen stimulates the secretion of chloride ions and water from the GIT wall. This lead to watery diarrhea. Dehydration and electrolyte imbalance lead to the death of the patient.
vii. Fermentation reactions: Ferment carbohydrates with release of acid and gas
1. Glucose: Positive
2. Maltose: Positive
Sucrose: Positive.
Mannitol: Positive,
Lactose: Negative
viii. Biochemical reactions
1. MR: Positive
2. Oxidase: Positive
3. Indole: Positive
4. Gelatin: Positive
5. Nitrate: Positive
6. Cholera red reaction: Positive
7. VP: Negative
8. Urease: Negative
9. Citrate: Negative
10. TSI
11. Base: Acid, Slant: Alkaline, No release of gas.
2. Antibiotics related to Vibrio cholerae: Sensitive to tetracyclines, ampicillin, streptomycin, kanamycin, etc.
3. Distribution of Vibrio cholerae: Human is a reservoir of Vibrio cholerae, fresh water, slightly salty water, see foods, warm coastal water, and sewage.


NEISSERIA
There are two medically important species of the genus Neisseria. These are Neisseria gonorrhoeae and Neisseria meningitides. Other species of the genus Neisseria are also present in the normal bacterial flora of the upper respiratory tract.
A. Neisseria gonorrhoea (gonococcus)
1. Characteristics of Neisseria gonorrhoea:
i. Gram-negative, aerobic, non-spore-forming non-motile cocci bacteria
ii. No polysaccharide capsule on Neisseria gonorrhoeae cells,
iii. The outer portion of a cell has protein that helps Neisseria gonorrhoeae to attach with host cells.
iv. Neisseria gonorrhoeae produces endotoxin.
v. Ferment glucose but cannot ferment lactose, maltose and sucrose.
vi. Habitat: Parasite of the human body.
vii. Pathogenicity: Infection in human body urinogenital tract, female rectum, pharynx, conjunctiva. Gonococcal infection may lead to gonococcal arthritis and ulcerative endocarditis.
viii. Culture media requirements: Enriched culture media eg. Chocolate agar culture media containing blood heated up to 80 degrees C. Heating destroys inhibitors present in the blood and carbon dioxide-enriched (5 to 10%) atmosphere. Optimum temperature 37o C. Incubation period 24 to 48 hours.
ix. Colony: Round, 1 to 3 mm diameter, slightly elevated lobbed edge, transparent, and greyish.
x. Biochemical Reactions: Oxidase positive and catalase positive,
xi. Fermentation Reactions: Only Glucose positive, lactose negative, maltose negative, sucrose negative.
2. Antibiotics related to Neisseria gonorrhea: Sensitive to penicillin, ampicillin, tetracycline, and several other antibiotics.
3. Distribution of Neisseria gonorrhea: Parasite of human body parts such as urinogenital tract(male and female) eye conjunctiva, pharynx, female rectum,
B. Neisseria meningitides (Meningococcus)
1. Characteristics of Neisseria meningitides:
i. Gram-negative, aerobic, non-spore-forming, non-motile cocci bacteria
ii. Occurs in pair (diplococci) with flat or concave surface on opposite side.
iii. They produce endotoxin that is chemically lipopolysaccharide.
iv. Ferment glucose but cannot ferment lactose, maltose and sucrose.
v. Habitat: Nasopharynx, bloodstream and meninges
vi. Pathogenicity: Infection in meninges, intravascular hemolysis, meningococcal arthritis.
vii. Culture media requirements: Enriched culture media e.g. chocolate agar culture media and carbon dioxide enriched (5 to 10%) atmosphere. Optimum temperature 37o C. Incubation period 24 to 48 hours.
viii. Colony: Round, 1 to 3 mm diameter, entire edge, slightly elevated, transparent or translucent, and shiny colony, waxy and become rubbery after 48 hours. The size of the colony in chocolate agar media is slightly bigger than the colony in blood agar media
ix. Biochemical Reactions: Oxidase positive and catalase positive.
2. Antibiotics related to Neisseria meningitides: Sensitive to penicillin, ampicillin, and cephalosporins.
3. Distribution of Neisseria meningitides: Human body Nasopharynx, bloodstream, and meninges
TREPONEMA PALLIDUM
It belongs to the family Spirochaetaceae. There are several species of the genus Treponema. Among them, a medically important species is Treponema pallidium.
1. Characteristics of Treponema palladium:
i. Elongated, motile, flexible anaerobic, and spiral or coiled bacteria.
ii. Not visible under an ordinary microscope. A dark field microscope is used.
iii. Not stained by normal bacteriological stains. Silver impregnation technique is used to stain it.
iv. Pathogenicity: T. palladium is transmitted through skin lesions or mucus membranes of the mouth, rectum, and genitalia. Sexually transmitted syphilis is called venereal syphilis. An infected woman transmits syphilis to the fetus after the third month of pregnancy. This is called congenitally acquired syphilis and non-veneral syphilis.
v. Culture: Not suitable artificial culture media is available. In complex fluid media under anaerobic conditions, it can survive for 10 to 14 days.
2. Antibiotics related to Treponema palladium: Penicillin is the antibiotic of choice to treat Treponema palladium infection i.e. syphilis.
3. Distribution of Treponema palladium: Human body genital area.
MYCOBACTERIUM
There are several species of the genus Mycobacterium. Among them, two are medically important Mycobacterium. These are Mycobacterium tuberculosis and Mycobacterium leprae. Mycobacterium tuberculosis causes the disease tuberculosis in the human body. Mycobacterium leprae causes leprosy in the human body.
A. Mycobacterium tuberculosis:
It causes tuberculosis in the human body. Other species of Mycobacterium such as M. bovis and M. africanum also cause tuberculosis in the human body.
1. Characteristics of Mycobacterium tuberculosis:
i. Non-motile, non-capsulated, non-spore-forming, aerobic, rod-shaped bacteria.
ii. Difficult to stain, but once stained by the Ziehl-Neelsen method, it resists decolorization. Hence called acid-fast bacteria.
iii. Microscopy by Fluorescent microscopy.
iv. Behaves like an obligate pathogen, an opportunistic pathogen, and saprophytes.
v. Habitat: Infected human body, dogs, and other animals.
vi. Pathogenicity: Pulmonary tuberculosis and non-pulmonary tuberculosis such as renal tuberculosis, urogenital tuberculosis, blood, tuberculosis, meninges tuberculosis etc.
vii. Culture requirements: Protein-rich culture media under aerobic conditions. Optimum temperature 37o C.
viii. Colony: Non-pigmented, light brownish yellow colored raised, dry, colonies,. Growth occurs slowly and may take 2 to 8 weeks.
ix. Microscopy: Stained by Ziehl-Neelsen method
x. Biochemical reactions
a. Niacin production test: Positive,
b. Nitrate reduction test: Negative,
c. Aryl sulphatase test: Negative,
d. Growth in thioacetazone: Negative.
e. Catalase peroxidase test: Positive.
Antibiotics related to Mycobacterium tuberculosis:
i. First Line Drugs: Isoniazid, Rifampicin, Ethambutol, Pyrazinamide, and Streptomycin
ii. Second Line Drug: Kanamycin, Amikacin, Cycloserin, Capreomycin, Viomycin, Thiacitazone, Ethionamide, Para-Amino Salicylic Acid (PAS), Quinolones.
Distribution of Mycobacterium tuberculosis: Infected human body, dogs, and other animals.
B. Mycobacterium leprae (Leprosy bacillus)
1. Characteristics of Mycobacterium leprae:
i. Non-motile, non-capsulated, non-spore-forming, aerobic, rod-shaped, slightly curved bacteria.
ii. Difficult to stain, but once stained by the Ziehl-Neelsen method, it resists decolorization. Hence called acid-fast bacteria.
iii. Habitat: Nose, upper respiratory tract,
iv. Pathogenicity: Affects skin and peripheral nerve.
2. Antibiotics related to Mycobacterium leprae: Dapsone, rifampicin, clofazimine,
3. Distribution of Mycobacterium leprae: Human body nose and upper respiratory tract.
Dr Pramila Singh
