Bone – marrow
Bone–marrow: Composition and function of bone marrow. Aspiration of bone marrow by various methods. Preparation, staining, and examination of bone marrow smears for myelogram including M.E. Ratio. Iron staining (Perls’ reaction). Significance of bone marrow examination.
Dr Pramila Singh
3/8/20249 min read
Bone–marrow: Composition and function of bone marrow. Aspiration of bone marrow by various methods. Preparation, staining, and examination of bone marrow smears for myelogram including M.E. Ratio. Iron staining (Perls’ reaction). Significance of bone marrow examination.
Composition and function of bone marrow
Bone marrow is a soft and spongy tissue found in the cavities of bones. It is a major component of the musculoskeletal system and is crucial for the formation and maintenance of blood cells. There are two types of bone marrow: red bone marrow (also known as myeloid tissue) and yellow bone marrow.
Red Bone Marrow: Most of the bone marrows in young individuals are red bone marrow. They are rich in blood vessels, hematopoietic (blood-forming) cells, and supporting stromal cells. Hematopoietic cells include various cell types, such as red blood cells (erythrocytes), white blood cells (leukocytes), and platelets (thrombocytes).
Yellow Bone Marrow: Yellow bone marrow is mostly present in the central cavities of long bones in adults. They contain more fat cells (adipocytes) and fewer hematopoietic cells than red bone marrow. They can transform into red bone marrow in certain conditions, such as severe anemia.
Normal ranges for differential counts on aspirated bone marrow/smear
1. Reticulocytes: 6.1 to 2%
2. Hemocytoblasts: 0.1 to 1%
3. Myeloblasts: 0.1 to 3.5%
4. Promyeloblasts: 0.5 to 5%
5. MYELOCYTES:
a. Neutrophils: 5 to 20%
b. Eosinophils: 0.1 to 3%
c. Basophils: 0 to 0.5%
6. METAMYLOCYTES
a. Stab forms: 10 to 30%.
7. POLYMORPHONUCLEARS
a. Neutrophils: 7 to 25%
b. Eosinophils: 0.2 to 3%
c. Basophils: 0 to 0.5%
8. Lymphocytes: 5 to 10%
9. Monocytes: 0 to 0.2%
10. Megakaryocytes: 0.1 to 0.5%
11. Plasma cells: 0.1 to 3.5%
12. Proerythroblasts: 0.5 to 5%
13. Normblasts:
14. Polychromatic: 2 to 20%
Pyknotic (Orthocromatic): 2 to 10%
Function of Bone Marrow:
The bone marrow is a dynamic tissue. It continuously produces blood cells. Its composition and function are tightly regulated to maintain circulatory and immune system homeostasis.
1. Hematopoiesis: The primary function of bone marrow is hematopoiesis. The formation and development of blood cells are called hematopoiesis. Hematopoietic stem cells (HSCs) in the bone marrow can differentiate into various blood cell types, such as red blood cells, white blood cells, and platelets.
2. Erythropoiesis: Red bone marrow is responsible for the production of red blood cells (erythrocytes). The formation of red blood cells is called Erythropoiesis.
3. Leukopoiesis: Bone marrow produces different types of white blood cells, such as neutrophils, lymphocytes, monocytes, eosinophils, and basophils. The formation of white blood cells is called Leukopoiesis.
4. Thrombopoiesis: Forming platelets in bone marrow is called thrombopoiesis.
5. Storage of Nutrients: Bone marrow stores various nutrients, including iron in association with hemoglobin production and calcium needed for bone health.
6. Fat Storage: Yellow bone marrow stores fat. It converts fat to red bone marrow during times of increased hematopoietic demand.
7. Cellular Support: Stromal cells in the bone marrow provide a supportive environment for hematopoiesis. These cells produce extracellular matrix and growth factors that regulate the development and function of blood cells.
Aspiration of bone marrow by various methods
Aspiration of bone marrow is the withdrawal of a sample of bone marrow for diagnostic or therapeutic purposes. The procedure is commonly performed from the posterior iliac crest (hip bone), the sternum (breastbone), or other bones. Bone marrow aspiration is often used to evaluate blood disorders, leukemia, infections, and other conditions. The following methods are used for aspiration of bone marrow.
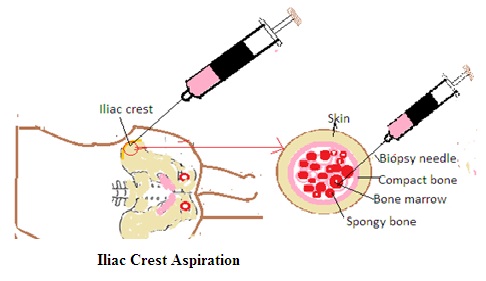
1. Iliac Crest Aspiration: This method is used for adult patients.
· Patient Positioning: The patient is usually placed in a prone (face-down) or lateral decubitus (side-lying) position. The main advantage is that the patient can not see what is happening. Several attempts at puncture and aspiration can be made.
· Site Selection: The posterior iliac crest is the most common site chosen for bone marrow aspiration. It is located on the back of the hip bone. It is an area that contains a large area of bone marrow. A relatively large volume of bone marrow can be aspirated from this area..
· Local Anesthesia: The skin over the chosen site is cleaned and numbed with a local anesthetic to reduce pain.
· Needle Insertion: A thin, hollow needle is inserted through the skin and into the bone. Allow needle penetration into the cortical bone to reach the marrow cavity.
· Aspiration: A syringe is attached to the needle. Bone marrow is aspirated into the syringe by applying negative pressure.
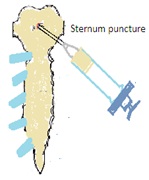
2. Sternum (Breastbone) Aspiration: This method is used for adult patients. It is preferred over the Iliac Crest Aspiration method. It is the ideal method due to the following reasons
i. The bone is near the surface.
ii. The cortical bone is thin and
iii. The bone marrow cavity in the sternum contains numerous cells of little fat.
Procedure
· Patient Positioning: The patient is usually placed in a supine (lying on the back) position.
· Site Selection: The sternum, specifically the sternal body, can be used as an alternative site for bone marrow aspiration.
· Local Anesthesia: Similar to iliac crest aspiration, the skin over the sternum is numbed with a local anesthetic.
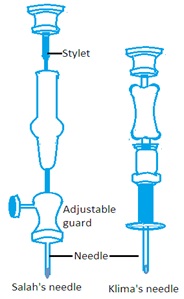
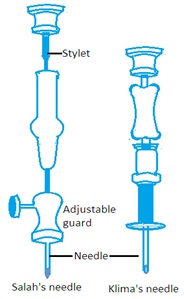
· Needle Insertion: A needle is inserted through the skin and into the bone marrow space. There are many types of needles but Salah’s needle and Klima’s needle are mainly used.
Methods of sterna puncture:
· Allow the patient to lie on a firm bed. The clean first and second pieces of sternum.
· Sanitize it using spirit iodine and again by spirit.
· Insert the needle in the midline of the sternum at the second interspace.
· When the needle is at the periosteum, anesthetize the area and push the needle further 5 mm.
· Push the needle with a boring motion into the bone cavity. Suck up not more than 0.3 mL of bone marrow material.
· Aspiration: Aspiration is performed by attaching a syringe to the needle and creating negative pressure to withdraw the bone marrow sample
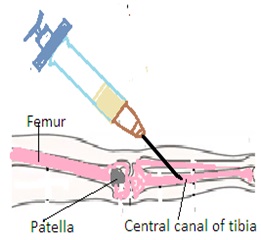
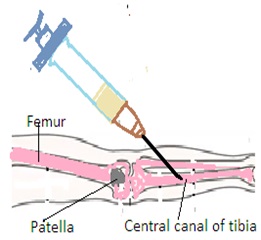
Tibial Aspiration: This method is used for infant patients.
· Patient Positioning: The patient is usually placed in a prone or lateral decubitus position.
· Site Selection: The tibia (shinbone) can be used as an alternative site for bone marrow aspiration, particularly in pediatric patients.
· Local Anesthesia: The skin over the tibia is numbed with a local anesthetic.
· Aspiration: The bone marrow sample is aspirated using a syringe attached to the needle
Post-Procedure Considerations
· After the procedure, pressure is applied to the site to minimize bleeding.
· The bone marrow aspirate is examined under a microscope to assess cell morphology, count, and other characteristics.
· Complications are generally rare but may include pain, bleeding, or infection at the aspiration site
Bone marrow aspiration is usually a well-tolerated procedure, and the choice of the site depends on factors such as the patient's age, the clinical indication, and the preference of the healthcare provider. It is essential to follow sterile techniques and proper safety measures during the procedure.
Preparation, staining, and examination of bone-marrow smear for myelogram including M.E. Ratio (Myeloid: Erythroid ratio).
A myelogram involves the preparation, staining, and examination of bone marrow smears to assess the cellular composition of the bone marrow. The myelogram is a valuable diagnostic tool used in the evaluation of various blood disorders, including leukemia, anemias, and other hematological conditions. It provides more useful qualitative information than time-consuming differential counts.
Preparation of Bone Marrow Smears for Myelogram
1. Patient Preparation: Obtain informed consent from the patient. Explain the procedure to the patient, addressing any concerns. Ensure that the patient's coagulation status is within normal limits.
2. Procedure: The bone marrow sample is typically obtained through bone marrow aspiration or biopsy. Smears are prepared on glass slides by spreading a small amount of bone marrow aspirate across the sterile and clean slide surface.
3. Staining of Bone Marrow Smears: Wright-Giemsa Stain is the most commonly used stain for bone marrow smears. It provides a multicolor stain that allows for the visualization of different cell types.
· The smear is flooded with Wright-Giemsa stain for a specific period.
· After staining, the slide is washed with buffer or water.
· The slide is then air-dried before microscopic examination.
Examination of Bone Marrow Smears
1. Microscopic Examination: The stained bone marrow smear is examined under a microscope. Different types of cells are identified based on their morphological characteristics, such as size, shape, and staining properties. Important cell types include erythroblasts, myeloblasts, lymphocytes, monocytes, and megakaryocytes.
2. Myeloid to Erythroid (M.E.) Ratio: The M.E ratio is based on counting 200 to 500 cells. The Myeloid to Erythroid ratio (M.E. Ratio) is calculated to assess the relative proportions of myeloid cells (such as myeloblasts and granulocytes) to erythroid cells (erythroblasts). An increased M.E. Ratio suggests a myeloproliferative disorder, while a decreased ratio indicates erythroid hyperplasia or other conditions affecting erythropoiesis.
Interpretation of Results
1. Cellular Composition: The myelogram provides information about the distribution and maturation of different hematopoietic cells in the bone marrow.
2. Cell Abnormalities: Abnormalities in cell morphology, such as the presence of immature cells (blast cells), abnormal cell shapes, or cytogenetic abnormalities are indications of various hematological disorders.
3. M.E. Ratio: An abnormal M.E. Ratio provides valuable information about the underlying pathology and guides further diagnostic workup.
4. Normal range: 2.5-15:1
Results from the myelogram are integrated with clinical and other laboratory findings to make a comprehensive diagnosis. The interpretation of bone marrow smears requires expertise in hematopathology or pathology.
Iron staining (Perls’ reaction).
Perls' Prussian blue reaction is a histochemical staining method. It is used to detect and visualize iron deposits in tissues. This staining technique is particularly useful in pathology to identify the presence of iron, as seen in conditions such as hemochromatosis, hemosiderosis, and certain anemias.
Perls' Reaction for Iron Staining
1. Reagents
· 2% Hydrochloric Acid (HCl),
· 2% Potassium Ferrocyanide Solution (Perls' Reagent),
· Nuclear Fast Red Counterstain.
2. Procedure
· Deparaffinization and Hydration: Deparaffinize and hydrate the tissue sections through a series of xylene and graded alcohol washes.
· Pearl’s Reaction: Incubate tissue sections in a 2% hydrochloric acid (HCl) solution for 20 minutes. This step enhances the reaction by removing loosely bound iron from the tissues. Rinse the sections in distilled water.
· Incubation in Pearl’s Reagent: Incubate the tissue sections in a freshly prepared 2% potassium ferrocyanide solution (Perls' reagent) for 30 minutes to 1 hour. This reagent reacts with ferric iron to form a blue precipitate (Prussian blue).
· Rinse: Rinse the sections in distilled water to remove excess Perls' reagent.
· Counterstaining: Counterstain the sections with Nuclear Fast Red for a short period (e.g., 5 minutes). This visualizes the cellular structures.
· Dehydration and Monitoring: Dehydrate the sections through a series of graded alcohols. Clear the sections in xylene. Mount the sections with a suitable mounting medium.
Result: Iron deposits will appear blue (Prussian blue) under the microscope, indicating the presence of iron in the tissue. Cellular structures are counterstained with Nuclear Fast Red, This develops contrast.
Perls' reaction specifically stains ferric iron, forming the blue Prussian blue complex. It does not stain ferrous iron. The reaction is sensitive and can detect even small amounts of iron deposits. Interpretation of results should be performed by a trained pathologist or histotechnologist. The intensity of staining and the distribution of iron deposits can provide information about the extent and nature of iron overload or deposition in tissues.
This staining method is a valuable tool in the diagnosis and characterization of various iron-related disorders and plays a role in understanding the pathophysiology of diseases involving iron metabolism.
Significance of bone-marrow examination
Bone marrow examination is a diagnostic procedure. It analyses of the soft and spongy tissue found in the cavities of bones, known as bone marrow. This examination provides valuable information about the health and functioning of the bone marrow, blood cells, and certain systemic conditions. It provides valuable information for clinicians to make accurate diagnoses, plan appropriate treatments, and monitor the progress of patients with blood disorders or related diseases.
The following are the significance of bone marrow examination.
1. Blood Cell Production: Bone marrow is responsible for the production of blood cells, including red blood cells (erythrocytes), white blood cells (leukocytes), and platelets (thrombocytes). By examining the bone marrow, doctors can assess the status of blood cell production and identify any abnormalities.
2. Diagnosis of Blood Disorders: Bone marrow examination is helpful in diagnosing various blood disorders, such as leukemia, lymphoma, myelodysplastic syndromes, and myeloproliferative disorders. Abnormalities in the number, size, or structure of blood cells can be detected through this examination.
3. Evaluation of Anaemia: Anemia is a condition characterized by a reduced number of red blood cells or a deficiency in hemoglobin. Bone marrow examination helps in determining the cause of anemia. This detects anemia due to decreased production of RBC, increased destruction of RBC, or other underlying factors.
4. Assessment of Infection: Bone marrow examination is used to investigate certain infections, such as tuberculosis or fungal infections. It provides information on the involvement of the bone marrow in the immune response to infections.
5. Staging and Monitoring of Cancer: The bone marrow examination is essential for staging the disease and monitoring the effectiveness of treatment of hematologic cancers like leukemia and lymphoma. It helps determine the extent of cancer involvement in the bone marrow.
6. Identification of Metastatic Diseases: The cancer cells from solid tumors can metastasize to the bone marrow. Bone marrow examination helps in the identification of these metastatic cells. This provides information about the spread of cancer.
7. Evaluation of Bone Marrow Disorders: Certain non-cancerous conditions affecting the bone marrow, such as aplastic anemia, myelofibrosis, and hemophagocytic syndromes are diagnosed and characterized through bone marrow examination.
8. Transplantation Planning: A thorough examination of the donor's and recipient's bone marrow is conducted to ensure compatibility and assess the health of the bone marrow before hematopoietic stem cell transplantation (bone marrow transplant).
Dr Pramila Singh
